Related Posts
Feb 27, 2026 7 mins read
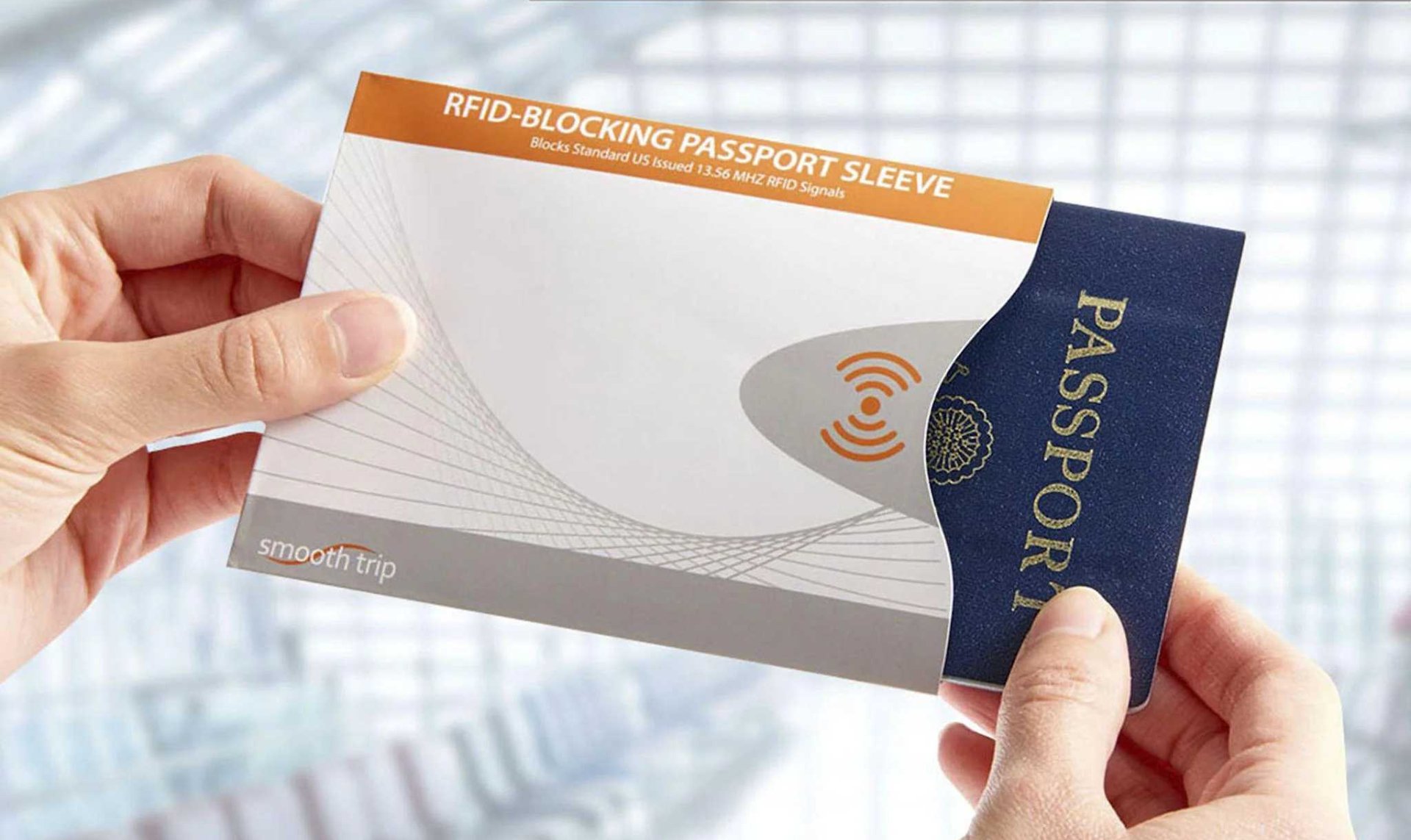
What Are the Best and Worst Safety Gadgets for International Travelers?

Feb 26, 2026 6 mins read
What’s New in International Hunting?

Feb 25, 2026 5 mins read
What Do Travelers’ New Year Resolutions Reveal About the Future of International Travel?

Feb 24, 2026 6 mins read
Is Spain the Best Value Destination in Western Europe for Culture and Travel?

Feb 20, 2026 6 mins read
What Are the Best Travel-Sized OTC Medications Every Traveler Should Pack?

Feb 19, 2026 5 mins read
What Do Most Travelers Get Wrong About International Travel Safety?

Feb 18, 2026 5 mins read
Which Countries Punish Online Speech and Photography, and How Can Travelers Stay Out of Trouble?

Feb 17, 2026 5 mins read
Inside Some of the Venues of World Cup 2026
Mobile Apps:
- Global Rescue Mobile Apps are designed for operation on the current versions of Android and iOS operating systems. Availability of services is subject to your equipment compatibility, connectivity and signal in your location. There is no guarantee that all features and functionality will be available in your location. Use and availability of the Mobile Apps are subject to your service provider’s plan and may be subject to additional fees from your provider. The download and use of a Global Rescue Mobile App is subject to the terms of your Member Services Agreement and the applicable End User License Agreement (EULA).
General TotalCare Disclaimer:
- ©2026 Global Rescue LLC. TotalCare and the TotalCare logo are service marks of Global Rescue LLC. All Rights Reserved. Global Rescue LLC provides technical and administrative services to Elite Medical Group, P.C. (“Elite Medical”), a professional corporation owned by licensed physicians that employs or contracts with physicians licensed to practice medicine where medical services are provided. It is not guaranteed that a prescription will be written, nor will any DEA controlled substances, non-therapeutic drugs and certain other drugs which may be harmful because of their potential for abuse, as a result of a TotalCare consultation. Elite Medical physicians reserve the right to deny care for potential or actual misuse of services. The Global Rescue Mobile App is designed for operation on the current versions of Android and iOS operating systems. Availability of services is subject to your equipment compatibility, connectivity and signal in your location. There is no guarantee that all features and functionality will be available in your location. Use and availability of the Mobile App is subject to your service provider’s plan and may be subject to additional fees from your provider.
Extended Plan TotalCareSM:
- For individuals 85+, medical transport is not included in membership. Members 85+ may purchase medical transport on a fee for service basis.
Mobile Apps:
- Global Rescue Mobile Apps are designed for operation on the current versions of Android and iOS operating systems. Availability of services is subject to your equipment compatibility, connectivity and signal in your location. There is no guarantee that all features and functionality will be available in your location. Use and availability of the Mobile Apps are subject to your service provider’s plan and may be subject to additional fees from your provider. The download and use of a Global Rescue Mobile App is subject to the terms of your Member Services Agreement and the applicable End User License Agreement (EULA).

