Categories:
Missions & Member TestimonialsMay 9, 2016
For the second consecutive year, Global Rescue sponsored and participated in the Boston Marine Corps Honor Run 5K, held on Saturday, May 7, 2016, at Carson Beach in South Boston. The event brought together approximately 1,000 participants, including civilians and active duty and veterans from all branches of the US Military and their families.
The Boston Marine Corps Honor Run 5K is organized in support of the Marine Corps Scholarship Foundation – the nation’s oldest and largest need-based scholarship program for military children, with a special commitment to supporting those whose parent has been killed or wounded in combat.
Global Rescue had a team of eight runners in the race, and was on site before and after the event, providing post-race refreshments for all participants.
Categories:
Health & SafetyTravelMay 4, 2016
Many people dread snakes – so much so that they actually avoid going outdoors to fish, hunt, hike, or picnic. Others out of a misplaced fear, will kill every snake they see.
As an outdoor enthusiast, it’s really only a matter of time before you will encounter a snake in the backcountry. Contrary to popular belief, snakes are not in the business of looking for people to bite.
Despite their sinister reputation, snakes are more afraid of you than you are of them. Most snakes do not act aggressively toward humans without provocation. Although many harmless snakes will bite to defend themselves, usually their bite produces nothing more than simple scratches.
With Global Rescue’s snake safety tips, you’ll be able to enjoy the outdoors and avoid direct encounters with snakes.
Venomous Snakes
Snakes are reptiles and like their relatives, lizards and crocodiles, they are legless, covered with scales, cold-blooded, can swim and have been around for millions of years.
All snakes eat other animals, while some snakes even eat other snakes. Snakes, even venomous ones, are important to the environment and help to control populations of rodents and other pests.
Only about 400 of 3,000 snake species worldwide are poisonous. These venomous snakes are most prevalent in temperate and tropical climates, with April-October being peak snakebite season. About 25 species of poisonous snakes are found in North America.
The Likelihood of Dying from a Snakebite
Though the exact number of snake bites is unknown, an estimated 5.4 million people are bitten each year with up to 2.7 million envenomations, according to the World Health Organization. Between 81,000 to 138,000 people die each year from snake bites, and around three times as many amputations and other permanent disabilities are caused by snakebites annually.
One in 37,500 people are bitten by venomous snakes in the U.S. each year. The chances of dying from a venomous snakebite in the United States are nearly zero, because of the high-quality medical care in the U.S.
The risk of dying from a venomous bite increases when multiple bites are involved and when the bite occurs in the young, old or among individuals with underlying respiratory or cardiovascular problems.
By contrast, a snake bite is the leading medical emergency in the Asia-Pacific, resulting in 46,000 deaths each year. Poor, rural areas that lack appropriate medical care and the correct antivenom contribute to this high number of snakebite fatalities.
Who Gets Bitten By Snakes?
In the United States, a significant number of people who are bitten by a snake are the ones who handle or attack snakes.
The majority of poisonous snakes in the U.S. are pit vipers. Rattlesnakes, copperheads and cottonmouth (water moccasin) snakes are in this family.
Typically, snake bite victims tend to be young males, between 11 and 19 years old, who are bitten on the hand while trying to pick up the snake.
People attempting to take a “selfie” with the snake are at high risk of being bitten. Dead snakes, even several hours later, can reflexively bite, causing either a second bite or biting another member of the group.
What Does a Snake Bite Look Like?
The Centers for Disease Control and Prevention offers a list of signs and symptoms, which include:
- Puncture marks at the wound
- Redness, swelling, bruising, bleeding, or blistering around the bite
- Severe pain and tenderness at the site of the bite
According to Medical News Today, a venomous snake bite will usually leave two clear puncture marks. In contrast, a nonvenomous bite tends to leave two rows of teeth marks. It can be difficult to tell, especially if the site swells immediately, so seek medical attention for any snake bite.
What to Do If a Snake Bites You?
Field management for snakebites should focus on limiting the systemic spread of the venom and rapid evacuation of the victim to a medical facility equipped to handle envenomations. While waiting for evacuation, do the following:
- Keep the patient calm and inactive. Remove jewelry and constrictive clothing.
- Clean around the bite site and keep the wound free from dirt and debris by covering with a sterile dressing.
- Immobilize the limb in a neutral position.
- Avoid the use of compression bandages unless bite is from a neurotoxic snake (coral snake, cobra, krait or other).
- Note the time of the bite and share with emergency staff.
For those with advanced medical training or wilderness emergency medicine training, monitor vital signs, ensure airway is unobstructed, and be prepared to treat victim for anaphylaxis, nausea, vomiting and pain.
How to Treat a Snake Bite
According to John Hopkins Medine, at the emergency department you may be given:
- Antibiotics to prevent or treat developing infections
- Medicine to treat your pain
- A special type of antivenin depending on the type of snake that bit you and the severity of your symptoms
As with any deep puncture to the skin, infection is a concern. The wound should be irrigated and cleaned at a hospital emergency department or emergency health clinic.
The person who is bitten by a snake may need a tetanus shot. Tetanus boosters should be given every 10 years.
Take Global Rescue with You
Wherever you travel, study your destination ahead of time. This may include researching the native flora and fauna that might be harmful.
If you plan on exploring off the road and into the tall grass, take a travel protection membership with you. Global Rescue memberships include personalized advisory services, 24/7/365 emergency assistance and evacuation services from the point of illness or injury. To learn more about membership benefits, click here.
Get a price estimate
Estimate
$0.00
Please answer all questions for estimate.
Categories:
NewsMay 4, 2016
Categories:
Health & SafetyApril 25, 2016
Malaria is found most often in Africa, Southern Asia, Central America, and South America, and is relatively rare in the United States. The disease is caused by a bite from a parasite-infected mosquito. Symptoms of malaria can include fever, chills, sweats, body aches, and muscle pain. Fever that goes away and returns is fairly common. Nausea, vomiting, abdominal pain, backache, and dark urine are also possible symptoms. More severe forms affecting mental status and organs typically require hospitalization. Left untreated, malaria can be fatal.
1. How do I know if malaria is an issue where I’m traveling?
For updated information on countries with malaria, use the resources available through either the Centers for Disease Control and Prevention (CDC) or the World Health Organization (WHO). Both of these organizations have maps with malaria risk levels indicated by country, and for regions within countries as well. Global Rescue members can contact Global Rescue for specific malaria advice, or can access country-specific information using the Global Rescue Mobile App. It is important to consider the time of year of your travel. If a country has malaria, there is usually some seasonality to it. Typically malaria follows the rainy season, and is particularly active in the middle to the late part of the rainy season when water is pooling in areas; standing water allows malaria-carrying mosquito larva to populate. Additionally, the more rural your destination, the higher the likelihood of malaria being a concern.
2. Who is at greatest risk?
Anyone who is not native to an area certainly faces an increased susceptibility to malaria. There is a level of tolerance that develops over time in those who are born and live in areas with malaria. A look at global statistics shows that greater than 75% of people who die from malaria are children under five years old. Weigh carefully any decision to travel with children to malaria-prone areas as they are the group that is most at risk for negative outcomes if malaria is contracted. The elderly are the next at-risk population, and the third class of traveler at an increased risk is pregnant women.
3. How can I protect myself?
Take precautions such as wearing long sleeves, using DEET repellants to ward off mosquitoes, and sleeping under netting. Most countries typically have mosquito nets in stores and even supermarkets, but if you’re concerned that you won’t be able to find them, it is a good idea to buy them in advance. The insecticide treated nets are best. People sometimes pre-treat their clothing, too. There are anti- malarial prophylactic medications (preventative therapies) that one can take. It is important to note, however, that none of these treatments is 100 percent effective. Seek advice from your regular healthcare provider, or a provider experienced in travel medicine to help decide which of these medications might be best for your individual health profile.
Again, it is always a good idea for travelers to check in with their primary care provider or a travel medicine professional before traveling for a detailed discussion of their risk for malaria.
Categories:
Missions & Member TestimonialsApril 14, 2016
Global Rescue’s Bryan Ody will be running the 2016 Boston Marathon on April 18, 2016, in support of the Martin Richard Foundation.
Bryan wrote on his fundraising page, “I am running the Boston Marathon this spring as part of TEAM MR8 for the Martin Richard Foundation. Martin was the 8 year old boy killed in the 2013 terrorist bombing of the Boston Marathon. Many can appreciate how terrorism and indiscriminate violence towards civilians has impacted our lives. As a retired veteran, this rings true more than most. I have chosen to fight against this violence by raising money in Martin’s name. Martin had a message of ‘No more hurting people. Peace.’ I will carry that message to the finish line.”
Bryan, a U.S. Army veteran who ran his first marathon in Taji, Iraq, is honored to represent the foundation and be part of one of the greatest marathons on earth. To learn more or to donate to the Martin Richard Foundation, please go to http://www.firstgiving.com/fundraiser/bryan-ody/bostonmarathon2016.

Categories:
Missions & Member TestimonialsApril 12, 2016
pictured: Julie Cook with Global Rescue Senior Specialist paramedic Justin Romanello (l) and Supervisor Kyle Bertrand (r).
The roads of Italy lead through thousands of years of history, presenting spectacular views and faithfully following the contours of rugged mountain terrain, while providing the ultimate challenge and potential for peril to motorcyclists.
“We knew going on this trip that those were the most dangerous roads to ride on in the world,” recalled Julie Cook. “That’s why we purchased Global Rescue. Thank God we did.”
It was the summer of 2015. Julie and her husband Eric were enjoying a tour through Europe on a new BMW R1200R as part of a small group led by a European motorcycle tour, where Julie is employed. “It’s a nice job perk, having the chance to take a tour that the company runs all over Europe. This year, we were riding through Slovenia, Czech Republic, Germany and Italy,” Julie said.
Then, on one of Italy’s tiny, winding roads, Julie and Eric’s motorcycle adventure took a sharp turn for the worse. Eric was driving and Julie was seated behind. It took only a split-second and suddenly the motorcycle fell off the road and flipped down the mountainside.
“I knew instantly that my leg was broken,” said Julie. “I could feel it and I heard it. I heard it break. I couldn’t move at all. Eric was able to move around – although he was in pain.”
Help on the way
The tour leaders acted swiftly and called for a local ambulance. “Eric pulled his membership card out of his jacket and called Global Rescue,” Julie said. He told them that both he and his wife were being transported to a hospital in Tolmezzo, Italy, for evaluation. “Both Eric and I immediately thought, ‘Thank God we have Global Rescue.’”
Upon initial assessment at the hospital, Julie was diagnosed with a lower right leg fracture. She was admitted to the hospital and scheduled to undergo a surgical repair of her leg the following day.
“It was difficult not being able to speak any Italian,” recalled Julie. “Once we were able to speak with Global Rescue, we knew that they had checked out the hospital and were doing everything possible to take care of us. It was such peace of mind.”
Global Rescue immediately deployed two paramedics to Julie’s bedside.
“I remember Eric saying that Global Rescue would be here soon and would begin to figure out a plan to get us home. Knowing that two Global Rescue people from the States were coming to help us get through this really helped me stay strong.”
When Global Rescue’s paramedics arrived, Julie greeted them with smiles and tears.
“It was a very happy moment,” said Julie. “All of my worries and all of the unknowns disappeared. The Global Rescue team took control of the situation and started making a plan to get me safely and comfortably back home. I will never forget how wonderful they were and how much they did to make my transport comfortable.”
Julie continued, “I felt so much relief once they explained how everything was going to happen, from beginning to end. They were on top of everything, including coordinating with hospital medical staff and sending my medical records to the Global Rescue medical team. When you’re injured, you just can’t deal with everything on your own. There’s no way my husband, who had torn ligaments in his knee, could have dealt with everything that happened.”

Julie with the Global Rescue team in Italy
Distraction by iPad
Boredom set in quickly for Julie with no landline in the hospital room, no international calling plan, no TV in the room and no air conditioning.
“When you’re going through that type of pain and you don’t have any way to distract yourself, it’s very difficult. One of Global Rescue’s paramedics said, ‘I have my iPad and I have some movies on it.’ He lent me his iPad, which was just the nicest thing. I was able to watch movies and take my mind off of everything for a while. If those Global Rescue guys had any way to help, they were there to help. They did everything they possibly could.”
The Global Rescue team accompanied Julie and Eric home. “I was happy to learn that I wasn’t going to have to fly home in a normal seat. They upgraded me to first class,” said Julie.
Back home
Once at home in New York, Julie faced a long recovery following multiple surgeries. She was instructed not to put any weight on her leg for three months.
“I had broken my tibia, my fibula, and I had a rod going down my leg and pins and screws holding it together. I had broken off the right hand side of my knee.”
Although confined to a hospital bed in her living room, Julie maintained a positive outlook. “I’m typically super healthy and active. Nothing gets me down. I’m always on the go and considered the healthy one. We have a wonderful family that keeps me company and brings me coffee. I’m feeling better now that this last surgery is over, knowing that I’m finally on my way to healing and getting better.”
Julie is unsure if another motorcycle trip will be in her future. “My husband probably would go,” she said. “We knew going on this trip that those were the most dangerous roads to ride on in the world. That’s why we purchased Global Rescue. Thank God we did. I’d probably still be in Italy because there was no way we could have afforded to be transported the way we were. We were lucky that we’d asked ourselves beforehand whether coverage was worth it. You just never know what can happen.”
“I cannot imagine how much pain and how many problems we would have had to endure without the help of Global Rescue,” said Julie. “We are so happy with Global Rescue. I will be recommending Global Rescue to all of our motorcycle tour clients.”
Categories:
Missions & Member TestimonialsApril 7, 2016
(Photo courtesy of Veristride)
Global Rescue CEO and Founder Dan Richards shared his views on the topic, “Teams Operating on the Edge of Human Performance” during Thin Air Park City in early April. Richards was part of a panel of elite athletes and executives discussing ways to optimize team dynamics and support to enable the full potential of human performance. The session followed opening remarks by Under Armor CEO and Founder Kevin Plank and Fortune Magazine’s Managing Editor Adam Lashinsky.
Joining Richards on the panel were Tiger Shaw, CEO of US Skiing & Snowboard Association; Paul Winsper, Vice President of Performance at Under Armour; Luke Bodensteiner, Executive VP of Athletics for USSA; and Richard LePage, Director of Coaching and Performance at Cirque du Soleil.
With a 2016 theme of “Innovation in Peak Human Performance,” Thin Air Park City gathers groups of inspired people to Park City, Utah, each year to solve business challenges and foster innovation.
Categories:
Missions & Member TestimonialsApril 7, 2016
Pictured: Global Rescue Associate Director of Medical Operations Devon Davis, MD (l), Geoffrey Corn, Missy Corn, and Global Rescue Supervisor of Medical Operations Patrick Longcore.
On safari in the Eastern Cape Karoo region of South Africa in January 2016, Global Rescue members Missy and Geoffrey Corn were having the time of their lives. It was their fourth trip to Africa and the couple was looking forward to creating memories of a lifetime. Little did they know that Missy was about to suffer a potentially life-threatening stroke on the first day of their trip, thousands of miles from home.
Global Rescue received a call from the outfitter for the Corns’ trip. The caller urgently stated that Missy was suffering from signs of a stroke — facial drooping, left arm and leg weakness, confusion, and speech difficulty.
With time of the essence, Missy was immediately transported to the hospital via ambulance after an evaluation by a local physician.
Preparing for the worst
Global Rescue Operations personnel immediately contacted the hospital, liaising with Missy’s physician there to discuss treatment. The company deployed one of its physicians and a critical care paramedic to Port Elizabeth to Missy’s bedside to oversee her care and later evaluate her stability for a flight back to a hospital close to home.
Upon arrival at the hospital, Missy underwent radiological studies showing an ischemic stroke and large arterial clot in the right brachial artery. She was admitted to the intensive care unit for care and observation. Subsequent radiology revealed progression to a hemorrhagic stroke but no other new brain injury.
While in South Africa, Global Rescue’s medical personnel helped to obtain Missy’s medical records for Global Rescue doctors to review. Through a consultation with Johns Hopkins Medicine, with which Global Rescue has an exclusive relationship, physicians there agreed with the Global Rescue medical team’s assessment and guidance on continuing medical care.
The Global Rescue team evaluated transport options. Determining Missy’s case to be critical, the team initiated an air ambulance to conduct medical repatriation back to her home hospital.
An unexpected delay
Then, a further complication: radiological studies of Missy’s lungs showed the presence of multiple pulmonary emboli, including the main pulmonary artery. The critical nature of her condition required cancelling the air ambulance evacuation based on the possibility of it proving fatal (the jet had traveled from Europe and was refueling in Namibia at the time the mission was scrubbed). With the presence of new clotting, an anticoagulation medication was needed. Yet, due to the previous discovery of bleeding in Missy’s brain, this medication could potentially cause further bleeding and also prove fatal.
With no other option, anticoagulation was initiated and she was transferred to the ICU for close observation.
After spending the weekend in the ICU and developing no new issues with the medication, Missy was transferred to the general ward. Over the next two weeks, she worked with physical therapy and our deployed personnel as she prepared for her return to the U.S.
Based on improvement in her condition and the physician’s recommendations, Missy was finally determined to be fit to withstand the long flight home after [another week] of rehab and stabilizing care. Global Rescue medical personnel identified a comprehensive stroke center in the Denver area, the closest suitable facility to the Corns’ residence.
Missy was discharged from the hospital to the care of Global Rescue paramedics, who accompanied her from the South African hospital to the facility in Denver, Colorado.

Missy Corn
A personal touch
Missy praised the Global Rescue paramedic who was at her bedside for weeks in South Africa.
“He knew everything that was going on medically with me and would explain it to me,” she said. “When I ended up back in the ICU, he came every day and kept track of me. He talked to my sisters and knew everything about my care and my doctor. When I didn’t know what was going on, he just handled it. Then when my husband left and I was there by myself, it was even more important to have him there.
She continued, “Anything I needed, he got it for me. He smuggled in blueberries because I was losing weight and couldn’t eat the food in the hospital. I broke out in a horrendous rash from the soap they washed me with, and he went and got me little bars of soap so I wouldn’t break out. He held my hand when I needed it.
“He was amazing, all that he did for me. If it weren’t for Global Rescue, I probably wouldn’t be here,” said Missy, emotionally.
Recovering back home
Upon arrival at the Denver hospital, Missy was transferred to the neurological unit for evaluation.
After a successful transport home accompanied by two members of Global Rescue’s transport team, Missy was able to continue her recovery. Following an evaluation in Denver, she was transferred to an inpatient rehabilitation facility in Kansas. In March, she was discharged to her home.
“I’m working therapy five days a week and I can walk without a cane now,” said Missy. “The fine motor skills in my left hand are coming back slowly. It’s not where I need to be yet, but I’m trying to get back into my daily routine.”
Missy is on track for a good recovery. In fact, she and her husband already have plans to return to South Africa in September if she is well enough. Once again, they will head out on safari.
“I tell all my friends and family that if they’re doing any travel, I recommend Global Rescue highly,” said Missy. “We purchased annual Global Rescue memberships this year and it was worth every penny.”
Categories:
NewsApril 6, 2016
Categories:
Health & SafetySecurity & IntelligenceTravelApril 4, 2016
There have been no documented cases of mosquito-borne transmission of Zika virus in the continental U.S. However, cases have been confirmed in people who have traveled to Zika-infected countries or acquired it through sexual transmission. According to the Centers for Disease Control and Prevention (CDC), between January 1, 2015 and March 30, 2016, at least 312 cases of travel-related Zika virus have been confirmed in the U.S., with the highest number of cases reported in Florida (74), New York (46), Texas (27) and California (17).
What areas are more susceptible?
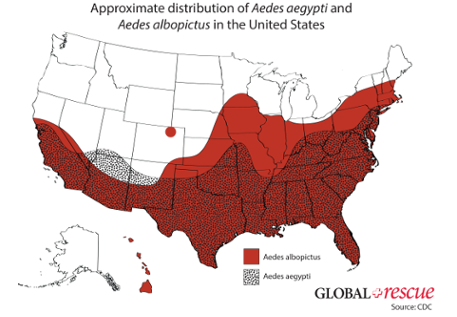
Although it is impossible to predict whether the virus will spread to mosquitoes in the U.S., sporadic small-scale outbreaks of dengue and chikungunya — similar tropical mosquito-borne diseases spread by the Aedesmosquito — have been reported in the past in south Florida and southern Texas. Some cities in the southeastern and eastern coastal regions of the U.S. might be more prone to Zika transmission due to established populations of Aedesmosquitoes. However, in order for local transmission to take place, the Zika virus would need to be introduced by an infected traveler or infected mosquitoes and become sustained in an established population of Aedesmosquitoes.
According to a National Institute of Health (NIH) study, about 200 million citizens — more than 60% of the U.S. population — reside in areas of the U.S. conducive to the spread of Zika virus during summer months due to the presence of Aedes mosquitoes. At least one of the two Zika spreading mosquitoes are found in 38 states from California, southeast to Florida, and northeast to Maine (see map below). The southern and southeastern regions of the U.S. from California along the Gulf Coast and up the eastern coast to Connecticut contain both the Aedes aegypti and the Aedes albopictus mosquitoes.
What conditions make Zika favorable?
Both the Aedes aegypti and the Aedes albopictus species of mosquitoes are known to spread Zika. The two species need warm and relatively stable temperatures to survive and standing water to reproduce.
Meteorological conditions favorable for the Aedes mosquitoes are not present in the U.S. during winter months from December to March, except for south Florida and southern Texas. However, weather conditions become more suitable for Aedes mosquitoes during peak summer months from July to September.
A March 2016 study conducted by the National Center for Atmospheric Research (NCAR) and the University Corporation for Atmospheric Research (UCAR) simulated climate data and other information such as mosquito populations, air travel from Zika-affected countries, and poverty to investigate the likelihood of Zika spreading in 50 U.S. cities.
According to the study, by mid-July meteorological conditions in southeastern cities will be suitable for “high abundance” of the Aedes, eastern cities will be suitable for “moderate to high abundance” and cities in western U.S. are suitable for “low to moderate abundance.” Cities most at risk are Miami, Orlando, Savannah and Charleston. Cities with moderate risk are New York, Philadelphia, and Washington, D.C.
What will help?
Public health experts say any outbreaks are expected to be small and short-lived due to the vastly different conditions from countries experiencing widespread transmission.
Many countries experiencing a rapid spread of Zika are poorer and lack adequate public health response capabilities, limiting their abilities to contain and combat the virus. For instance, in countries where air conditioning is not commonly used and/or screens are not widely used on windows and doors, people are exposed to open air (and mosquitoes) for longer periods of time, allowing the virus to spread more easily.
Conversely, in the U.S., well-built homes, screened windows, air conditioning and access to mosquito preventative products are likely to limit or even prevent the spread of the virus.

What else should I know about Zika virus?
Zika virus is an acute viral illness primarily transmitted through the bite of an infected Aedes species mosquito that has previously fed on a person infected with the Zika virus. Zika can also be transmitted from mother to fetus, through blood transfusion, and through sexual contact.
The most common symptoms of Zika are fever, rash, joint pain and conjunctivitis. However, symptoms are usually mild and only last from several days to a week. About 80% of people infected do not experience symptoms. There is currently neither a vaccine nor a cure.
Prior to 2015, local transmissions of Zika virus had largely been confined to Africa, Southeast Asia and the Pacific Islands. Zika was first discovered in Uganda in 1947 and only 14 cases were confirmed from 1947 to 2007, all of which occurred in West Africa and South Asia. In 2007, the first outbreak was reported in Oceania when more than 185 cases were confirmed in the Yap Islands, an island chain in the Federated States of Micronesia. The virus then appeared in October 2013 in French Polynesia.
In May 2015, an outbreak of the virus began in Brazil and by April 2016, 34 countries and territories in the Americas reported local transmission of the virus. The recent outbreak of Zika has been strongly linked to birth defects, including microcephaly, an abnormal smallness of a newborn’s head associated with incomplete neurological development. The incidence of Zika has also been correlated to an increase in cases of Guillain-Barré syndrome, a syndrome in which the body’s immune system attacks part of the peripheral nervous system, causing paralysis.
In May 2015, the Pan American Health Organization (PAHO) issued an alert regarding the first confirmed Zika virus infection in Brazil and in February 2016, the World Health Organization (WHO) designated the Zika virus as a global public health emergency requiring a coordinated response, placing the disease in the same category of concern as Ebola. It is expected that Zika virus transmission will increase throughout the region increasing the incidence of infection in returning travelers and the possibility of local transmission in the U.S.
To stay up to date on Zika virus developments, contact us at 617-459-4200 or memberservices@globalrescue.com